Personal Injury: Where the Biopsychosocial Model Comes Alive
Why Trauma-Based Care Demands More Than “Treatment as Usual”
Personal injury (PI) doesn’t sit on the edges of healthcare.
It sits dead center.
Personal injury is not a niche, a side hustle, or an inconvenient category of patients. It is a core segment of trauma-based healthcare. And yet, far too often, PI patients are approached as “treatment as usual”—the same protocols, the same narrow focus, the same region-specific mindset.
Neck equals neck care.
Low back equals low back care.
Shoulder equals shoulder care.
I respectfully submit that this approach is a mistake.
Not just for your personal injury patients, but for your overall approach to trauma-based healthcare.
And more than almost any other category of care, personal injury demands a biopsychosocial model and approach.
The Biological Injury: What You’re Trained to See
Every personal injury case begins with a biological injury.
There is tissue damage.
Inflammation.
Loss of function.
Physical pain.
This is the physical trauma you are trained to recognize, diagnose, and treat. It’s the entry point of care and the most visible part of the injury.
But in PI cases, the biological injury often runs deeper than what’s initially obvious.
Undiagnosed concussions are common. Mild traumatic brain injuries—TBIs—are frequently missed.
And secondary injuries develop due to altered movement patterns, guarding, and compensation.
Yet, even when you do a good job addressing the biological injury, the injuries don’t stop there.
That’s where many providers unintentionally fall short.
The Psychological Injury: What Pain Changes
Personal injury almost always carries a psychological injury.
If you’ve ever been in a significant auto collision, you don’t need a textbook to understand this. You feel it.
Fear to get behind the wheel again.
Anxiety re-living the traumatic event and the fallout.
Hypervigilance.
Sleep disruption.
Loss of confidence in your body and what you can and can’t do.
Many PI patients experience undiagnosed post-traumatic stress disorder, or PTSD. Not because they’re “weak,” but because trauma rewires how the brain processes safety and threat.
Add to that the stress of the legal system.
Uncertainty about timelines.
Uncertainty about finances.
Uncertainty about the outcome.
Pain doesn’t just hurt. It changes how people think, move, and behave.
It affects treatment compliance.
It affects recovery speed.
It affects trust.
Ignoring the psychological component doesn’t make it go away. It simply makes treatment less effective.
More importantly, missing out on this segment means you may have missed out on key diagnoses and the timeliness of key specialist referrals. When missed, not only can your patient’s healthcare outcome be negatively impacted, but your own exposure to potential medical malpractice may also be increased.
Alternatively, handling this second segment right, in particular, can set you apart from your peers as a PI value-driver moving you to a PI specialist instead of a replaceable professional vendor.
The Social Disruption: What No Imaging Study Shows
And then there’s the most overlooked layer of all: the social impact.
Personal injury disrupts life, fast and hard.
Patients miss work or lose income.
Finances become strained.
Family dynamics shift under stress.
Transportation becomes a challenge.
Childcare responsibility becomes a barrier to injury care.
Appointments aren’t missed because patients don’t care.
They’re missed because life has been turned upside down.
Their normal routine ends overnight, replaced by uncertainty, with no clear finish line.
This social disruption affects:
- Treatment consistency
- Recovery length and even outcomes
- Emotional resilience
- Long-term health decisions
And yet, it rarely shows up in traditional documentation.
This is a key area for explaining away gaps in treatment. If there was truly a treatment gap, it may have been for these real life, explainable social impact reasons. And addressing them again elevates you to a PI value driver. A true PI and trauma-based healthcare pro.
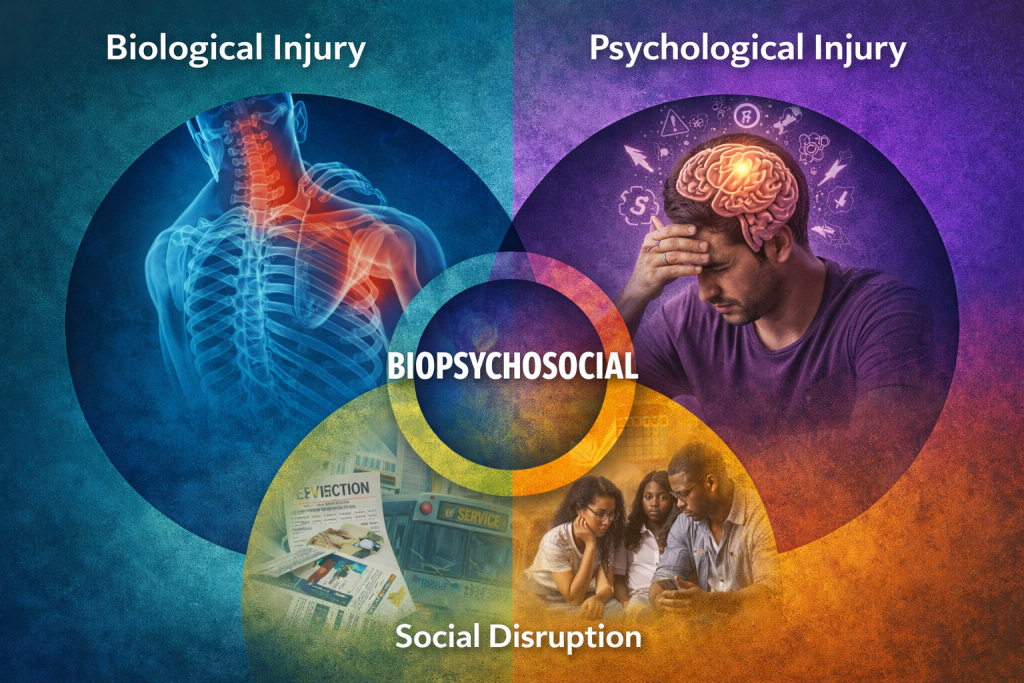
The Biopsychosocial Model in Real Time
This is the biopsychosocial model playing out in real life.
Biological injury.
Psychological injury.
Social disruption.
Each layer influences the others.
This is why PI care—and frankly, all healthcare—should be about treating the whole person, not just the symptom that brought them through the door.
A biopsychosocial approach doesn’t replace good clinical care. It elevates it.
What a Biopsychosocial PI Approach Looks Like in Storytelling Documentation
It starts with evaluating the entire body, not just the chief complaint.
It includes awareness of mental and emotional stressors without trying to play therapist.
And it never forgets that a patient’s social reality affects treatment plan compliance and healing.
This means your storytelling documentation evolves.
You still document pain, but you don’t stop there.
You document:
- Functional limitations
- Behavioral changes
- Work restrictions
- Sleep disruption
- Difficulty with activities of daily living
You go further.
You note:
- Duties performed under duress
- Loss of enjoyment of life
- How stress, finances, or transportation affect treatment
- How the patient’s unique life situation impacts recovery
This isn’t fluff.
This is clinically relevant, legally meaningful, and medically accurate healthcare storytelling.
Why This Aligns with Modern Healthcare
When PI is done right, it aligns perfectly with modern, evidence-based healthcare.
The biopsychosocial model is not fringe medicine. It’s widely accepted across pain science, rehabilitation, behavioral health, and trauma care.
PI care isn’t “extra.” It’s not “outside the system.”
It is trauma-based healthcare where biology, psychology, and social reality collide.
And this is where good medicine doesn’t just show up, it’s also where it matters most.
Your Opportunity as a Provider
You have an opportunity in personal injury.
Not just to treat injuries, but to be a difference-maker to your patients, the attorneys, your peers, judges and juries, and even yourself.
A provider who understands trauma.
A provider who sees the whole patient.
A provider whose evaluation, approach, treatment and documentation reflect reality, not just anatomy.
When you apply a biopsychosocial approach to PI care, you don’t just improve outcomes, you increase your value.
Personal injury is not a problem to tolerate.
It’s the perfect place for the biopsychosocial model to do what it does best—Deliver better care, better outcomes, and better medicine.